Targeting a key immune cell driver in lung fibrosis
When scar tissue builds up in the lungs, it becomes difficult to breathe easily. New research shows that a specific cell in the immune system [invariant natural killer T cell or iNKT for short] plays a vital role in how lung fibrosis develops. This may open the door to new therapies for this chronic disease.
There are approximately 1000 people in Ireland today living with idiopathic pulmonary fibrosis (IPF). The exact cause of IPF is not known, making it extremely difficult to develop drugs to treat the disease. The existing treatments only slow the progress of the disease.
An international research collaboration led by Conway Fellow, Professor Adam Byrne from UCD School of Medicine, is studying the role of iNKT cells to determine if blocking these cells would be useful to treat lung fibrosis.
The research team found increased numbers of iNKT cells in IPF-airways, compared to healthy volunteers. This suggests that the immune cell plays a specific role in the development of lung fibrosis. Then, using a drug to prevent the iNKT cells from working in their laboratory model of IPF, the team were able to reduce the disease in a preclinical model.
Commenting on the research findings, Professor Byrne said, “This particular type of immune cell has been shown to drive fibrosis in several other tissues. This work is significant because it reveals a previously unknown mechanism involving iNKT cells in the development of lung fibrosis.
The drug we tested in this study has now advanced to a phase 2 clinical trial where it will be evaluated in patients with IPF. We hope that this drug can eventually be used to treat IPF, which would have a profound impact on patients’ lives.”
The research study is published in the scientific journal, American Journal of Respiratory and Critical Care Medicine. The collaboration study also involved researchers from Imperial College London, University of California San Diego and the University of Southern California. The research was funded by GRI Bio.
Journal Reference
Emily Calamita*, Lauren Liu*, Patricia P. Ogger, Christina Michalaki, Albert Agro, Marc Hertz, Clare M. Lloyd, Philip L. Molyneaux, Vipin Kumar*, Adam J. Byrne*. Type 1 invariant natural killer T cells drive lung fibrosis. American Journal of Respiratory and Critical Care Medicine, https://doi.org/10.1164/rccm.202402-0288LE
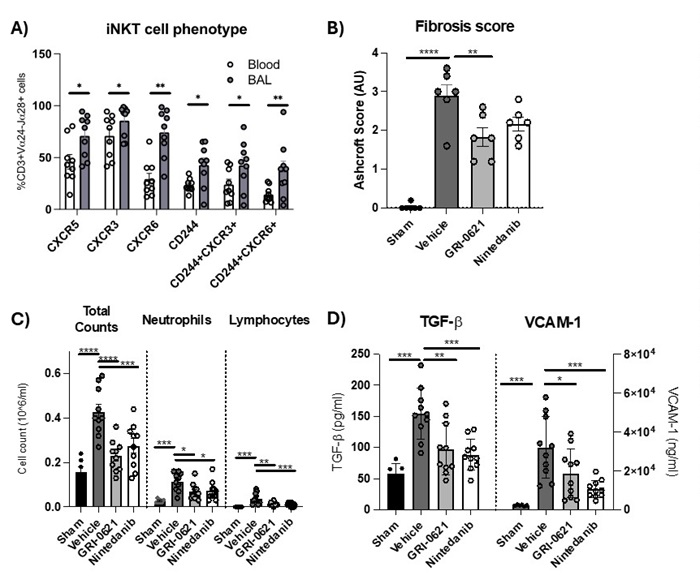 Figure 2: Proportion of Vα24-Jα18+ iNKT cells expressing CXCR5, CXCR3, CXCR6, CD244, co-expressing CD244 and CXCR3, co-expressing CD244 and CXCR6, in matched blood and BAL of IPF patients (n=9). Data presented as mean ± S.E.M. Statistical significance tested using a Wilcoxon test. *P < 0.05, **P < 0.01. (B) Ashcroft scores in mice. C) Total cell counts and numbers of neutrophils and lymphocytes in lung. D) Levels of TGF- and V-CAM in lung homogenates. n = 10-12 per group, pooled from two independent experiments. Data presented as mean ± S.E.M. Statistical significance tested using a Mann-Whitney’s U test. *P < 0.05, ** P < 0.01, *** P < 0.005, **** P < 0.001.
Figure 2: Proportion of Vα24-Jα18+ iNKT cells expressing CXCR5, CXCR3, CXCR6, CD244, co-expressing CD244 and CXCR3, co-expressing CD244 and CXCR6, in matched blood and BAL of IPF patients (n=9). Data presented as mean ± S.E.M. Statistical significance tested using a Wilcoxon test. *P < 0.05, **P < 0.01. (B) Ashcroft scores in mice. C) Total cell counts and numbers of neutrophils and lymphocytes in lung. D) Levels of TGF- and V-CAM in lung homogenates. n = 10-12 per group, pooled from two independent experiments. Data presented as mean ± S.E.M. Statistical significance tested using a Mann-Whitney’s U test. *P < 0.05, ** P < 0.01, *** P < 0.005, **** P < 0.001.
Social Media Links