Dr Brendan Kelly has shared his team’s latest research in AI and radiology. The new study shows the power of deep learning in making personalised predictions from radiographs. See a summary of the findings here.
Dr Kelly says, ‘’Our work can enable more accurate personalised predictions in colonic transit studies and potentially other  applications where change assessment is critical such as cancer treatment response and screening programs.
applications where change assessment is critical such as cancer treatment response and screening programs.
This approach opens a promising avenue for applying time series methods in radiology, an area where computer vision has previously been dominant. We've proved it's possible, and now we hope to see it used more widely.’’
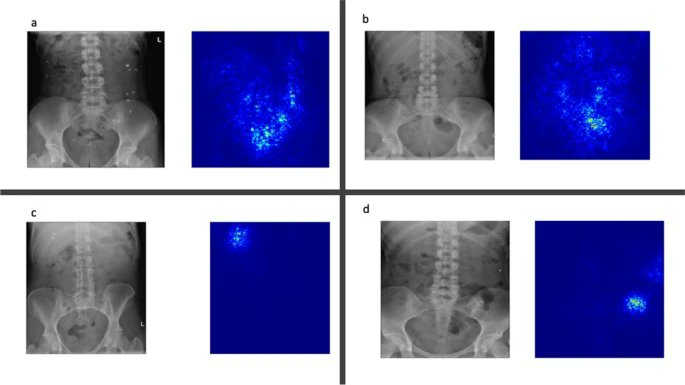
The team used Siamese Neural Networks in their research to classify the presence of radiopaque beads in colonic transit time studies. Simply put, they utilised a type of AI to analyse radiographs and pinpoint key elements.
They trained their SNN model on real-world patient data from 2010 to 2020. By using deep learning, their model could identify presence, absence, and count of beads with remarkable accuracy, precision, and recall of 0.988, 0.986, and 1 respectively.
However, they are not just identifying beads. Their model could also predict the total duration of the study using these findings as input and found that it outperformed conventional Gaussian process regression (GPR) models and statistical curve fitting methods.
Specifically, the MAE (Mean Absolute Error) of their model was 0.9 days, compared to 2.3 and 6.3 days for the GPR model and statistical curve fitting respectively. This is a statistically significant improvement.
The team also used Saliency Maps and PCA to give an intuition about how their model was acting.
Congratulations to Dr Kelly and his team, including Supervisors Dr Ronan Killeen (Radiology) and Assistant Professor Aonghus Lawlor (Computer Science).
This work was performed within the Irish Clinical Academic Training (ICAT) Programme, supported by the Wellcome Trust and the Health Research Board (Grant No. 203930/B/16/Z), the Health Service Executive National Doctors Training and Planning and the Health and Social Care, Research and Development Division, Northern Ireland and the Faculty of Radiologists, Royal College of Surgeons in Ireland. This research was supported by Science Foundation Ireland (SFI) under Grant Number SFI/12/RC/2289_P2.