A comprehensive review of Adverse Event Rates in Interventional Radiology
Wednesday, 2 October, 2024
Share

 Congratulations to final year Graduate Entry Medicine (GEM) student Aren Mnatzakanian, who is first author on a recently published paper in Springer Nature, in the journal Cardiovascular and Interventional Radiology (CVIR). Aren authored the paper with UCD School of Medicine's Professor Colin Cantwell (SVUH/UCD).
Congratulations to final year Graduate Entry Medicine (GEM) student Aren Mnatzakanian, who is first author on a recently published paper in Springer Nature, in the journal Cardiovascular and Interventional Radiology (CVIR). Aren authored the paper with UCD School of Medicine's Professor Colin Cantwell (SVUH/UCD).
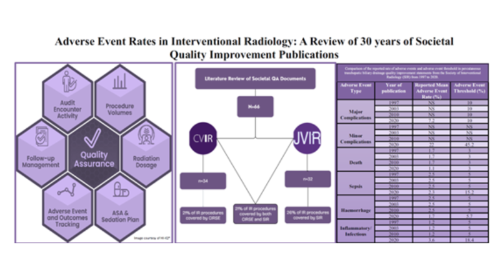
The paper is titled (opens in a new window)Adverse Event Rates in Interventional Radiology: A Review of 30 Years of Societal Quality Improvement Publications and Aren highlights the significance of the research stating, ''There is a critical need for renewed understanding of the governance process for adverse events within interventional radiology (IR). Quality improvement guidelines report adverse event rate ranges and suggested thresholds for specific complications in IR. We reviewed the available thresholds relevant for adverse event meetings in IR units and provided a practical searchable index resource for quality assurance. There is a need for additional guidance and support from IR societies to facilitate meaningful standardised reporting of adverse events and validate continuous quality improvement projects for IR units to implement in order to reduce adverse events.''
Congratulations to Aren and Prof Cantwell.
Introduction
 The care that interventional radiology (IR) provide should be effective, safe, and people-centred. In order to reassure patients, referring physicians, and regulators of the delivery of this high-quality care, IR departments are expected to implement a comprehensive quality assurance (QA) strategy and quality improvement (QI) programme.
The care that interventional radiology (IR) provide should be effective, safe, and people-centred. In order to reassure patients, referring physicians, and regulators of the delivery of this high-quality care, IR departments are expected to implement a comprehensive quality assurance (QA) strategy and quality improvement (QI) programme.
Quality is tracked by measurement of key performance indicators including patient safety, patient experience, and procedure outcome. These three outcomes are considered independently but they are codependent, for example, a patients’ experience and the effectiveness of a treatment are negatively impacted by lapses in patient safety. This article focusses on the available guidance on adverse event rate in IR procedures.
In order to facilitate an interventional radiology quality programme, the two main societies of interventional radiology, the Society of Interventional Radiology (SIR) and the Cardiovascular and Interventional Radiology Society of Europe (CIRSE), have published a framework of QA, QI guidelines and standards of care documents for specific procedures that report the range of complication rates, define threshold rates of complication for investigation, and guide acceptable practice.
The first quality assurance guideline in IR was published in 1995 by the SIR [(opens in a new window)1]. A multidisciplinary team led by recognized experts in the field was appointed by the Standards of Practice Committee to conduct a comprehensive literature search to identify studies regarding outcomes of the radiology procedure of interest. Data regarding the range of adverse event rates were extracted from relevant studies, and QA thresholds for adverse events were derived from a calculation of two standard deviations above the mean adverse event rate in the selected papers, or using a modified Delphi technique to achieve an 80% or greater consensus agreement on the threshold when the evidence in the available literature was weak, conflicting or contradictory.
The calculated adverse event thresholds are used in QA to detect outlying performance of an individual interventional radiologist. QA focuses on poorly performing individuals or low-quality events. In a system using an adverse event rate threshold of two standard deviations above the mean, 2% of the population of interventional radiologists will be identified in breach of the threshold adverse event rate and subjected to further investigation. The other 98% of interventional radiologists who have an adverse event rate below the threshold will be under no obligation to change their practice.
In quality assurance, no significant effort is focused on continuous improvement of interventional radiology technique, process, or patient care. The concept of a minimal standard of performance is reinforced, and a sense of “good enough” prevails. This “good enough” mentality is a disservice to patients in an era of ever-advancing health care.
QI on the other hand is a continuous cyclical process focused on reducing adverse events with an intervention. QA does not necessarily lead to quality improvement. Examples of effective validated quality improvement projects that reduce adverse events in IR are rare beyond procedural checklists. In surgery, reported successful QI projects focus on antibiotic use as the intervention in order to reduce infectious adverse events of surgery.
For the full paper, click (opens in a new window)here.